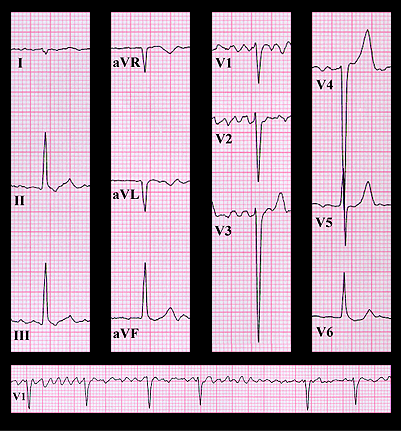
The ECG reveals atrial fibrillation and a frontal plane axis that is directed slightly to the right (+95 degrees). There is poor R wave progression in the V leads, and deep S waves in leads V3 and V4. The transition of the QRS complex from a dominant S wave to a dominant R waves occurs in lead V5 rather than in leads V3 and V4, where it normally occurs, suggesting clockwise rotation of the heart within the mediastinum. These changes are consistent with acute left ventricular dilatation. There is also slight ST depression in lead V6 which is probably due to the digitalis. In this previously asymptomatic patient, the sudden onset of symptoms, combined with atrial fibrillation, the described ECG changes and a loud apical systolic murmur that radiates to the back, are suggestive of acute mitral insufficiency,. The most likely diagnosis is a ruptured chordae tendineae. This diagnosis was confirmed and the chordal rupture was repaired.
